Clinical trials are one of three medical cannabis access pathways for legal cannabis in Australia. And, as cannabinoid medicine becomes more popular, more Australians want to learn about or take part in clinical trials.
While patients keep hearing from doctors and regulators that there isn’t enough clinical evidence about cannabis and medical conditions, there are many clinical trials being run at any given time. In this article you’ll learn about the clinical trial process, why clinical trials are important and how you can get involved. If you want to learn who can participate and how, you can skip to the end of the article from the index. Here’s what we cover with Melissa Benson in the interview:
General Clinical Trials Information
- 00:22 | What exactly is a clinical trial?
- What types of clinical trials are there for cannabis?
- 01:18 | Interventional studies
- 02:32 | Observational studies
- 03:05 | Why are clinical trials so important for medical cannabis?
- How does a trial on a mouse or rat help us understand medications on humans? (NEW VIDEO)
- 04:00 | What conditions do medications need to meet to be ‘clinically proven’?
- 05:18 | How many registered (clinically proven) medical cannabis drugs are there?
- 06:17 | How many cannabis clinical trials are there currently?
- 07:11 | Why is it so difficult to get large scale interventional cannabis trials?
- 09:32 | How do intellectual property issues impact research?
Australia Specific Information
- 11:29 | How does observational data play a part in cannabis access and reform?
- 12:40 | How does what’s happening overseas impact Australia?
- 15:16 | Are there any really notable Australian cannabis clinical trials?
- 17:18 | Ways to stay informed about cannabis clinical trials.
- 18:35 | Who can take part in clinical trials?
- 18:49 | Healthy people
- 19:13 | Patients or individuals with medical conditions
- 20:07 | What if there isn’t a current trial that suits me?
Note: At the time of recording there was only one medical cannabis drug, Sativex, listed on the ARTG. In September 2020 Epidyolex was added to the ARTG as an approved medicine.
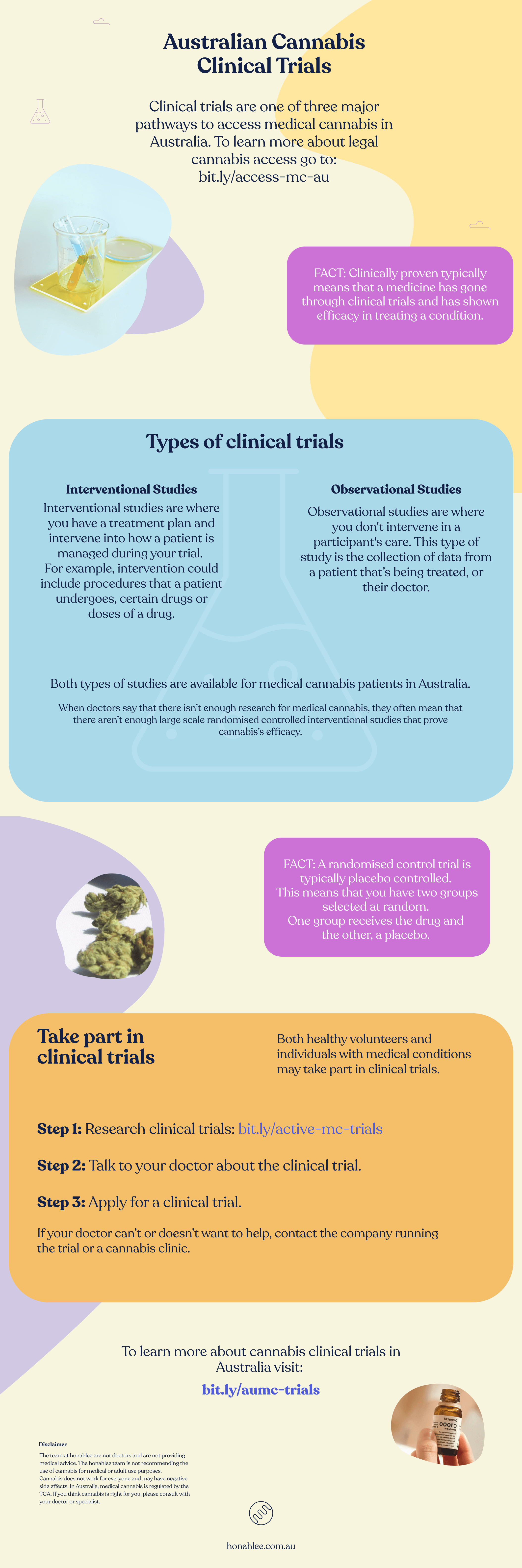
If you’d like an overview of what clinical trials are and how you can get involved, check out the infographic below.
What exactly is a clinical trial?
A clinical trial is an experiment that helps give you an answer to a research question. In the cannabis field, the question you may ask is, “How does cannabis help with inflammation?”
A clinical trial consists of:
- A measure for the test
- A control group
- A test group
For example, the measure could be swelling. The test group gets cannabis and the control group gets a placebo (a substance with no therapeutic effect). At the end of the test period you look to see if there was a difference in swelling between the two groups.
If there is a difference and statistical significance, a result from the experiment that is not likely to occur randomly or by chance, you have found your answer.
What types of clinical trials are there for cannabis?
There are two main types of clinical trials: interventional and non-interventional (aka observational studies).
Interventional studies
Interventional studies are where you have a treatment plan and intervene in how a patient is managed during your trial. For example, intervention could include procedures that a patient undergoes, certain drugs or doses of a drug.
An example of an interventional study is a randomised controlled trial (RCT). RCTs are the gold standard of clinical trials and are what doctors are referring to when they say “cannabis research” or “cannabis evidence”.
A randomised control trial is typically placebo-controlled or controlled by an active comparator. Controlled simply means that you have two groups selected at random and one group receives the drug and the other placebo.
Non-interventional (observational) studies
Observational studies are where you don’t intervene in a participant’s care. This type of study is the collection of data from a patient in treatment or from their doctor. This is happening with large cohorts of medical cannabis patients across the globe. Patients are being treated by a clinic or an independent physician and researchers collect data from both patients and their doctor for analysis.
Why are clinical trials so important for medical cannabis?
Clinical trials allow us to prove, scientifically, if a drug affects a particular condition. Clinical trials address three key areas of medicine:
- Safety – trials review the side effects patients are reporting and drug-drug interactions with the test drug and any other drugs a patient might be taking.
- Efficacy – trials look at how effective is the drug on the condition.
- Dose – they also help us understand doses or dosage ranges that a patient might need for efficacy.
What conditions do medications need to meet to be ‘clinically proven’?
In a traditional pharmaceutical sense, a drug is clinically proven in Australia when it’s registered on the Australian Register of Therapeutic Goods (ARTG). In order to be registered, you need to provide evidence to show that the drug is: safe and effective.
Safe and effective means that the trial has demonstrated an understanding of toxicity limits of doses of the drug and how frequently patients can have the drug. There’s an understanding of the expected adverse events and the side effects of the drug.
Finally, the trial must have proven the drug is effective for treating the condition tested. That can be against a placebo or against another drug on the market. For example, suppose you’re looking at antidepressants. In that case, the evidence must show that the drug your testing is better than an existing antidepressant, or that it’s as good as a current antidepressant or has a better side effect profile.
To be listed on the ARTG, a drug typically goes through four of the five phases of clinical trials. To learn about the five phases of clinical trials watch this video:
NOTE: Medical cannabis is an unapproved medicine (not listed on the ARTG) in Australia. The high financial outlay and amount of time that it takes to run clinical trials is one of the reasons that the potential framework for the down-scheduling of CBD means very little in its current form.
How many registered (clinically proven) medical cannabis drugs are there?
In Australia there are two medicinal cannabis products registered. There is Sativex, which is a one-to-one CBD to THC spray registered for the treatment of multiple sclerosis pain and spasms. There is also Epidyolex, a Cannabidiol (CBD) product to treat seizures associated with Lennox-Gastaut syndrome and Dravet syndrome, in patients two years of age and older.
How many cannabis clinical trials are there currently?
The number of clinical trials is growing daily.
If you look at the TGA guidance documents, which explain the thinking behind medical cannabis being legalised, the TGA looked at over 350 different studies about half of which were randomised control trials. There are also multiple trial registries. The largest local registry is the Australian and New Zealand Clinical Trials Registry. When you search the registry, you often find over a hundred trials running at any given time.
Why is it so difficult to get large scale interventional cannabis trials?
Melissa explained that it most likely comes down to financial motivation and intellectual property. Traditionally pharmaceutical companies create novel molecules to register for treatment of a specific condition. Those molecules can be protected with a patent. A patent gives you about 20 years of protection for that product or idea where no one else can impede upon the novel idea.
The protection gives a company time to go through the phases of clinical trials and when registered, these companies have five to 10 years of market share.
Cannabis is very different because you are not allowed to patent a naturally occurring compound. Companies can’t just patent CBD. So, there’s not an ability to capture all of the money you spent on large scale studies because you can’t get market exclusivity. So, if a company were to spend huge sums of money, many other products would likely be able to piggyback on the research completed.
While there are a couple of cannabis drugs patented, cannabinoid patenting is still very new and complex.
How do intellectual property issues impact research?
The lack of large scale trials impedes the growth of the medical cannabis industry because clinicians will continue to say there’s not enough evidence. Australian GPs tell their patients that there isn’t enough research on a daily basis. Scientists and many doctors want large studies, but don’t have a mechanism to fund them.
I think we’re trying to put an old framework onto a new problem, and no one’s really providing a solution as to how we’re going to overcome this. It seems very unlikely that regulators will, all of a sudden, not require this level of evidence. We need to find a way to be able to get the standard of evidence in a way that isn’t going to send a company bankrupt just because they want to try and fulfil this burden of evidence.
How does observational data play a part in cannabis access and reform?
Observational research is key. Observational research before having a medicine listed is very unique; because in a traditional pharmaceutical sense, you could never do observational research because your drug isn’t allowed to be prescribed.
In Australia, for example, we have over 18,000 patients receiving medicinal cannabis. So we have a large cohort where we could already be collecting important observational research.
And, we are doing just that. Several observational trials are happening Australia-wide. The problem is that observational studies are not the same quality or the same control level. However if we can create extensive data sets, they will be powerful. This is because they can become a bartering chip to say it’s our only option unless the government can facilitate other types of large scale studies or provide other solutions.
How does what’s happening overseas impact Australia?
While the TGA looks at the rest of the world, mainly the European nations and the FDA for guidance, Australia is on the forefront of cannabis research. While it may be easy to get low dose CBD products in the UK, for example, getting a script is even more complex than in Australia.
The US is an odd example where cannabis has been legalised in many of the states, but is still federally illegal. Because of these differences, US research has been hindered greatly. So even though it looks like their patient access is much stronger, it’s quite seperate to what’s actually happening in the research setting. Australia actually does a lot of research for overseas companies.
Are there any really notable Australian cannabis clinical trials?
Australia has done a lot of work on cannabis and driving. While not necessarily important for a specific condition, they are very important for all cannabis patients.
Driving with any THC in your system is illegal in Australia. But, the big question is at what level and time after consumption does cannabis impair driving? So for patients who need cannabis with THC to treat a condition like chronic pain, not being able to drive legally can increase anxiety or reduce quality of life.
There’s also another group in Melbourne called the Origin Youth Centre for Mental Health. A team of psychologists and psychiatrists primarily treat patients between the ages of 15 and 25 for refractory or treatment-resistant anxiety or treatment resistant depression and addiction.
Ways to stay informed about cannabis clinical trials.
The ANZ clinical trial registry is a great resource but isn’t as patient friendly as it could be. So, the team at Applied Cannabis Research (ACR) have created a database of current studies running in Australia. The database is a resource for patients to find Australian cannabis studies and link directly to many of those studies.
It’s also important for patients to note that there are opportunities in some of the observational studies to be done via telehealth.
Who can take part in clinical trials?
So there are two groups of people that can be involved in medicinal cannabis clinical trials. Both healthy and patients, or individuals with medical conditions, can be involved.
Healthy volunteers
Healthy volunteers are needed for a number of different types of studies. For example, in the cannabis and driving trials healthy volunteers were used. There are also pharmacokinetic studies which look at drugs and how they distribute throughout the body that may need healthy patients.
Those with medical conditions
If you’re a patient with a medical condition it’s best to start with your doctor. If you find a trial you would like to be a part of you can bring that to your physician. A clinical trial may be a good entry pathway to becoming a medical cannabis patient.
Whether you’re already a patient or a new potential patient, there are a number of observational studies that you might be able to partake in. There are also studies specific that certain indications like insomnia or chronic pain.
What if there isn’t a current trial that suits me?
ACR also recognised that there aren’t always trials running for the medical conditions that patients would be able to get involved in. To help patients, ACR created an online expression of interest form so that they can keep patients up to date on new trials or trials that might suit each patient.
Conclusion
In conclusion, clinical trials are crucial for the future of the medical cannabis space. While we need more large randomised controlled trials, they will be slow and few and far between. Until then, observational studies will continue to run and will offer doctors, researchers and the TGA data in the meantime.
If you’d like to search for clinical trials to take part in you can visit the ACR listing of clinical trials.
Understanding the clinical trials running and talking to your doctor about these opportunities are another way to show them cannabis is an accepted form of treatment. We hope you found this article helpful and wish you the best in your pursuit of medical cannabis.
Cannabis Clinical Trials Infographic